Streptococcus pyogenes (Group A Strep (GAS)
- Bacterial pharyngitis
- Flesh Eating disease (Necrotizing Fasciitis)
- Rheumatic/Scarlet Fever
Streptococcus agalacatiae – Group B Strep (GBS)
General Description
The Streptococci (strep) are Gram-positive bacteria, round in shape, which tend to form chains when seen in a Gram stain. There are two main human pathogens that are classified by a grouping method (Lancefield’s grouping) which are Group A Streptococci and Group B Streptococci.
Group A Streptococci Significance
Streptococcus pyogenes or Group A strep (GAS) is a common cause of upper respiratory and skin infections. People may also carry GAS in the throat or on the skin with no symptoms of illness. In the United States, more than 10 million non-invasive GAS infections, primarily throat and superficial skin infections, occur annually. Most GAS infections are relatively mild illnesses such as pharyngitis (strep throat) or impetigo (a skin infection). GAS can account for 15-30% of cases of pharyngitis in children and ~10% of cases in adults. Occasionally this bacteria can cause severe and even life-threatening diseases such as Streptococcal toxic shock syndrome (STSS), and Necrotizing Fasciitis (NF) – or “flesh eating” disease. STSS and NF each accounted for approximately 6-7% of cases. Other complications include Rheumatic and Scarlet Fever. Some strains are more deadly, based on the GAS cell wall proteins.
Group B Streptococci Significance
- agalacatiae or Group B Strep (GBS) disease is most common in newborns. In adults, most cases of GBS disease are among those who have other medical conditions. Other medical conditions that put adults at increased risk include:
- Diabetes
- Heart disease
- Congestive heart failure
- Cancer or history of cancer
- Obesity
Symptoms – GAS
GAS pharyngitis (sore throat) is usually a rapid onset sore throat with fever and pain with swallowing, without cough or runny nose.
GAS impetigo (Skin infection) will start with red bumps, which become pustules which then break to form crusty lesions.
Necrotizing fasciitis (NF) usually starts with swelling, redness, tenderness and heat at the site of infection. The pain felt is usually out of proportion to the signs of a skin infection. There may or may not be signs of a wound, and any progressive swelling, or ulcers, blisters or block spots on the skin needs to be investigated immediately. Also, dizziness, fatigue diarrhea or nausea can be experienced.
Streptococcal Toxic Shock Syndrome (STSS) begins with influenza like symptoms of fever, chills, muscle pain, nausea and vomiting. These symptoms can rapidly lead to sepsis with low blood pressure rapid heartbeat and breathing, failure to produce urine, yellowing of eyes, and signs of other organ failure.
Scarlet fever is characterized by a red rash usually with a GAS pharyngitis. It is most common among children 5 through 15 years of age. It is rare in children younger than 3 years of age.
Rheumatic fever develops if GAS pharyngitis or Scarlet fever is not treated promptly. It can present with a fever, joint pain, symptoms of heart failure, and fatigue.
In the pre-antibiotic era, streptococci frequently caused significant morbidity associated with significant mortality rates. However, in the post-antibiotic period, diseases due to streptococcal infections are well-controlled and not a common cause of death.
Symptoms – GBS
Colonized mothers will show no symptoms of having GBS, it is usually found by screening the vagina during pregnancy.
Newborns can present with early-onset disease (EOD – 0-7 living days) or late-onset disease (LOD – 7 days to 3 months). Symptoms can include fever, difficulty feeding, irritability or lethargy (limpness or hard to wake up the baby), difficulty breathing, or a blueish color to skin. Meningitis, pneumonia and sepsis can occur if left untreated.
Transmission – GAS
GAS is highly communicable and can cause disease in healthy people of all ages. The organism is commonly spread through contact with droplets from an infected person’s cough or sneeze, or mucus from the nose or throat. In addition, the spread may occur through contact with infected skin lesions or contaminated surfaces and sharing of utensils. Infected persons are most likely to spread the infection. The bacteria may be spread with contact of a person without symptoms but who carry the bacteria in their throat or on their skin (asymptomatic carrier). The individuals that have no symptoms are much less contagious. Although it is possible to spread these bacteria by drinking from the same glass or eating from the same plate as someone who is ill with a GAS, this is less likely to occur.
The incubation period for pharyngitis is 2-5 days. 24 hours after appropriate antibiotic therapy has been started, children can return to the daycare or school environment and adults can return to work.
Multiple streptococcal infections in the same family are common. Impetigo and pharyngitis are more likely to occur among children living in crowded homes and in suboptimal hygienic conditions.
Transmission – GBS
Transmission of GBS in adults can be through skin to skin contact or sexual contact. In the USA, there is little evidence of transmission between adults from food, water or common surfaces outside of healthcare.
Newborns will acquire GBS from their mother. The risk in increased with prolonged rupture of membranes, and passage through the birth canal.
Treatment
There is no vaccine against GAS or GBS, but the infection can be treated with antibiotics. To date, strep infections have remained universally susceptible to penicillin. Therefore, penicillin remains the first-line drug of choice for pharyngeal infections, as well as for complicated or invasive infections or prenatal infections. Physicians must be aware and concerned about the potential for life-threatening complications presented by infection with GAS. Even seemingly minor infections (e.g., pharyngitis, impetigo) may lead to fatal STSS. Treatment of NF (necrotizing fasciitis) requires surgical removal of the infected tissue in addition to antibiotics.
Prevention
The spread of all types of Streptococcal infections can be reduced by good general hygiene, including hand washing, especially after toileting, coughing, sneezing and before preparing foods or eating. People with sore throats and fever should be seen by a doctor who can perform tests to find out whether the illness is strep throat or a more systemic infection. If the test result shows strep throat, the person should stay home from work, school, or daycare until 24 hours after taking an antibiotic. All wounds should be kept clean and watched for possible signs of infection such as redness, swelling, drainage, and pain at the wound site. A person with signs of an infected wound, especially if fever occurs, should immediately seek medical care. It is not necessary for all persons exposed to someone with an invasive GAS infection (i.e., NF or STSS) to receive antibiotic therapy to prevent infection. That decision should be made after discussing with your doctor.
Vaccination against chickenpox and influenza can help, as GAS infection can be a complication of both viruses.
Cleaning and Disinfection
Diligent and frequent cleaning and disinfection of the environment is a key component in a comprehensive prevention strategy. This strategy is especially important to preventing the spread of infections especially in crowded areas such as schools, daycare centers and long term care facilities. The organism can survive on surfaces for up to 6.5 months.
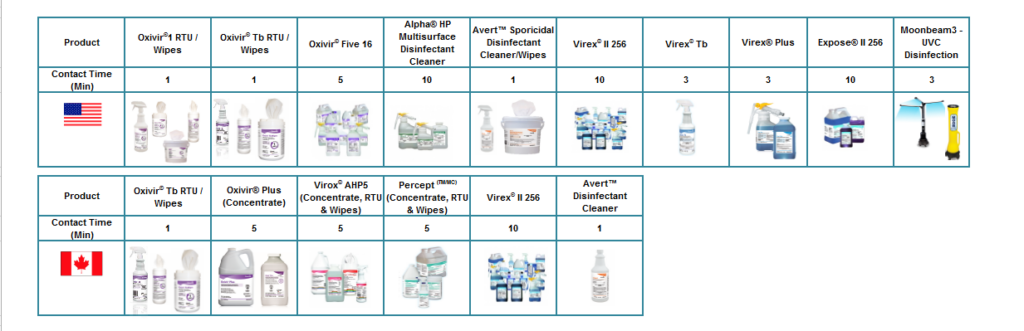
The Streptococci are Gram positive bacteria and the following Diversey products are effective against Gram positive bacteria:
References:

