General Information
Measles is caused by a single-stranded, enveloped, RNA virus with 1 serotype. It is classified as a member of the genus Morbillivirus in the Paramyxoviridae family. Humans are the only natural hosts of the measles virus and the virus is not transmitted to animals.
Measles is an acute, highly communicable, vaccine-preventable viral respiratory illness. It is characterized by a high fever (as high as 105°F) and malaise, along with the three “C”s: cough, coryza, and conjunctivitis. The rash usually appears on average about 14 days after a person is exposed. The rash spreads from the head to the trunk to the lower extremities. Patients are considered to be contagious from 4 days before to 4 days after the rash appears. Of note, sometimes immunocompromised patients do not develop the rash.
Significance
Measles was officially eliminated in Canada in 1998 and in the US in 2000, meaning there was no measles spreading within the country and new cases are only found when someone contracts measles abroad and returns to the country. Being vaccinated is the best way to prevent getting sick with measles or spreading it to others. There has been a resurgence of measles worldwide including in the US and Canada. The global COVID-19 pandemic has led to delays in surveillance and immunization efforts and vaccine hesitancy.
For the most up to date information on measles cases and outbreaks:
In the US: CDC Measles Cases and Outbreaks
In Canada: Health Canada Measles and Rubella Weekly Monitoring Reports
Measles is a reportable public health condition in both the United States and Canada, and suspected cases should be reported through local public health channels as soon as possible. Healthcare providers should notify their facility’s infection prevention and control team as well.
Symptoms
Symptoms of measles usually begin 10–14 days after exposure to the virus. A prominent rash is the most visible symptom.
Early symptoms usually last 4–7 days and include runny nose, cough, red and watery eyes, and small white spots inside the cheeks.
The rash begins about 7–18 days after exposure, usually on the face and upper neck. It spreads over about 3 days, eventually to the hands and feet. It usually lasts 5–6 days before fading.
Most deaths from measles are from complications related to the disease and include blindness, encephalitis (an infection causing brain swelling and potentially brain damage), severe diarrhea and related dehydration, ear infections, and severe breathing problems including pneumonia.
Measles can be serious in all age groups. However, children younger than 5 years of age and adults older than 30 years of age are more likely to suffer from measles complications.
Transmission
Measles is one of the most highly communicable infectious diseases with greater than a 90% secondary attack rate among people who are susceptible. The measles virus spreads through the air when a person who is infected breathes, coughs, sneezes or talks. It may also spread through direct contact with fomites or secretions from the nose and throat of a person who is infected. The incubation period is typically 11–12 days from exposure to the virus until the first symptoms appear.
People with confirmed measles are infectious from 4 days before rash onset to 4 days after the appearance of the rash. The measles virus can persist in the air or on surfaces for up to 2 hours after a person who is infected has left the space.
Airborne precautions should be used in healthcare settings for patients with confirmed or suspected measles.
Diagnosis
Healthcare providers should suspect measles in a patient presenting with:
- Febrile illness and rash
- History suggesting that the patient is not immune to measles especially if the patient has travelled or is known to have an epidemiologic link to a measles case or outbreak
Adequate specimens should be taken to diagnose measles. These include nasopharyngeal or throat swab, blood specimen and urine specimen. Tests include serology and RT-PCR.
Prevention
A measles vaccine is the best way to prevent measles. This vaccine is included in the combination measles-mumps-rubella (MMR) and measles-mumps-rubella-varicella (MMRV) vaccines. Two doses are recommended with one dose 93% (range: 39% to 100%) effective at preventing measles and two doses 97% (range: 67% to 100%) effective at preventing measles.
In addition to vaccination, follow these steps to help prevent illness:
- Wash your hands often with soap and water or clean your hands with hand sanitizer (containing at least 60% alcohol)
- Avoid touching your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing
- Try to avoid close contact, such as kissing, hugging, or sharing eating utensils or cups, with people who are sick
For infection prevention and control guidelines related to measles in healthcare settings refer to:
In the US: Interim Infection Prevention and Control Recommendations for Measles in Healthcare Settings
In Canada: Health Canada Measles for Health Professionals
Environmental Cleaning and Disinfection
Diligent and frequent cleaning and disinfection of environmental surfaces is a core strategy for the prevention and control of all infections. Measles is an enveloped virus, therefore, easy to inactive on environmental surfaces using an EPA or DIN approved disinfectant for use in healthcare or one that has been tested for efficacy against measles. Clean and disinfect frequently touched environmental surfaces and shared equipment per manufacturer’s instructions for use.
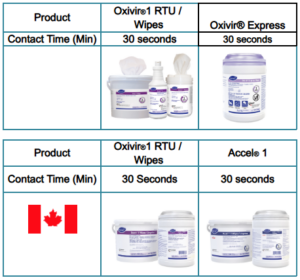
Measles is susceptible to the following Diversey disinfectants:
References:
CDC: https://www.cdc.gov/measles/hcp/clinical-overview/index.html
Health Canada: https://www.canada.ca/en/public-health/services/diseases/measles/health-professionals-measles.html
World Health Organization: https://www.who.int/news-room/fact-sheets/detail/measles

