KISS in Cleaning and Disinfection – Keeping it Simple, Safely

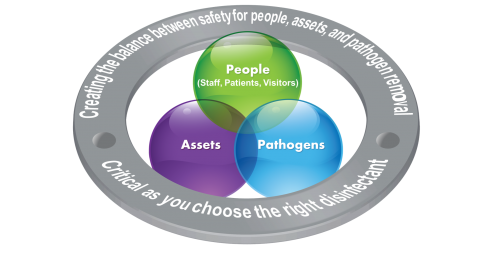
The ultimate goal of cleaning and disinfecting environmental surfaces is to create a safe environment for patients, their visitors, and healthcare personnel.
Environmental Services (EVS) and Infection Prevention (IP) departments continue to face the challenge of preventing the transmission of healthcare-associated pathogens (HAPs). Accomplishing this task can be difficult. There is increased pressure to make sure environments are safe. Infection rates are now reported, public awareness is much higher, and facilities face financial pressure from new reimbursement models. With the emergence of more multi-drug resistant organisms, effective cleaning and disinfection may seem like the last line of defense to prevent the spread of infection.
Many organizations are taking additional or extraordinary measures to address their issues. Several organizations have invested in “new” technologies, such as UVC and fogging, which promise “pathogen-free” environments. Others are making decisions to incorporate sporicidal disinfectants throughout their facilities as a precautionary measure. These investments have demonstrated varied results.
Here is a key question to consider. Do you have a standardized cleaning and disinfection protocol that is consistently practiced? Before taking extraordinary measures, one must consider whether the basic cleaning and disinfecting foundation is in place. Healthcare-Associated Infections (HAIs) continue to be a challenge in healthcare facilities, and addressing the basics may be the key to achieving consistent and improved results. There are many variables that can impact the spread of infection, but what we know for sure is that hand hygiene and environmental cleaning and disinfection are two of the keys to prevention. Maybe it is time to get back to the basics.
Unfortunately, many facilities lack a simple, systematic approach to improving environmental hygiene. Directors of EVS departments continually face significant reductions in staffing and budgets, and also a high rate of staff turnover. Prevention and operational efficiency can seem like conflicting goals, but with a clear plan they can both be accomplished.
Infection Prevention. Simplified.
Creating a simplified approach to environmental hygiene requires three key steps:
1) Assessment, 2) Selection and 3) Execution
1) Assessment: The first step in achieving this goal is to perform a facility-wide infection prevention risk assessment. Each facility needs to step back and assess their needs based on infection rates, pathogens of concern, and their current processes.
The most commonly feared pathogens in healthcare are Clostridium difficile, Carbapenem resistant Enterobacteriaceae (CRE), methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), and norovirus. These HAPs are either Gram positive or Gram negative bacteria or small non-enveloped viruses; of which only C. difficile is spore-forming.
As more pathogens become resistant to multiple antibiotics, there also seems to be a desire to have these resistant organism strains on disinfectant labels. It is noteworthy to mention that most disinfectants are effective against vegetative bacteria regardless of the antimicrobial resistance profile. There is no evidence that resistance to antimicrobials correlates with the effectiveness of disinfectants. This is due to fundamental differences in the mechanism of killing of microorganisms by these agents (antibiotics vs. disinfectants).
Once this assessment is completed, the next step is to select the appropriate disinfectants and tools to meet your facility’s needs.
2) Selection: To keep it simple, one disinfectant should be selected for daily cleaning of all patient rooms. This product should be effective against the pathogens of concern, and safe for use for patients, staff and visitors.
It may be necessary to select a specific task disinfectant, such as a sporicidal, for terminal cleaning of rooms that were occupied by C. difficile patients, or for enhanced cleaning during outbreaks. Sodium hypochlorite-(bleach) based disinfectants are most commonly used to address bacterial spores, but newer technologies are emerging.
Bleach is known to have deleterious impact on surfaces, including corrosion and pitting of equipment and other surfaces over time, and can cause employee related concerns such as the triggering of respiratory difficulties in workers using bleach-based solutions. Therefore, the use of bleach should be limited to outbreak situations of C. difficile and some non-enveloped viruses as recommended by the CDC. The physical removal of pathogens during proper cleaning and disinfection activities, along with the use of routine germicides can remove and dilute spore concentrations, and is an acceptable method in the absence of an outbreak.
The new “improved hydrogen peroxide” disinfectants are effective against all vegetative bacteria, enveloped viruses and the majority of non-enveloped viruses with various dwell times, including norovirus. The key benefits of improved hydrogen peroxide disinfectants are they act quickly, are odorless, and are safe on most surfaces. Unlike quats, they don’t exhibit binding activity to cleaning tools, which is known to decrease the efficacy of quat disinfectants.
An additional, and critical, consideration should be the risk of use on the health of patients, their families, and healthcare personnel. Healthcare personnel appreciates using products that are safe and effective. Finally, one must understand the effect that disinfectants can have on facility assets, such as furniture, personnel uniforms, and medical equipment.
3) Execution: There is strong evidence that proper cleaning and disinfection is critical to reducing the risk of transmission of pathogens. Most facilities focus their efforts only on terminal cleaning of patient rooms with less emphasis on daily cleaning. This must change in order to achieve better patient experiences and satisfaction. More emphasis should be placed on daily cleaning of frequently-touched surfaces, with a safe and effective disinfectant to reduce the risk of pathogen transmission. Frequently-touched surfaces include surfaces near the patient or those surfaces that are touched by many people throughout the day, such as light switches, bed rails, phones, door handles, etc.
Most importantly, facilities need to implement programs to measure and ensure that high touch surfaces are being cleaned effectively.
In summary, the key is making sure you have the basics covered. This starts by understanding your needs followed by selecting the right disinfectant. The disinfectant must be effective against key pathogens of concern, get the job done within realistic contact times, and not sacrifice the safety of your patients, visitors, staff or surfaces. Most importantly, creating a culture of DAILY cleaning and disinfection of high touch surfaces to reduce the bio burden and risk of hand contamination along with a thorough-and-consistent process for terminal cleaning of patient rooms will create positive results.
Keep it simple & safe (KISS)
These steps will go a long way toward creating a safer environment for patients, their families, and healthcare personnel.

